Short reverberation time does not do the whole trick in healthcare facilities, it´s the peaks that will wake the patients up!
Out of our comfort zone
When we are sick and feel bad – we seem to forget that just opening the door to a hospital makes us out of our comfort zone. Our system is already stressed and our senses therefor alert. We are more sensitive to sound and noise than normal – and in hospitals this can be a challenge.
Florence Nightingale in Notes on Nursing, 1859[1]:
Unnecessary noise is the most cruel absence of care which can be inflicted upon either the sick or well!
A lot of patients have been sick and well since then – but how do our patients feel about noise in a modern hospital today? From 2012-2017 a group of specialists from Sweden[2] focused on sound environments in the Intensive Care Unit (ICU) patient room to find out how critically ill patients are affected by sound and what can be done to improve the sound environments.
Sound levels (SPL) in the ICU
The group found that the average SPL in the ICU was 53 dB. You can of course discuss if 53 dB really is that loud. Isn’t it possible to sleep if the background noise has that limit? It would be like people talking from a distance but not near your head? Like a TV in your living room?
The problem with analyzing the average SPL is that people react more to peaks – and it is the peaks that will wake you up when you try to sleep. Average actually don’t tell us much in regards to human perception (when it is not harmful to the hearing – and 53 dB is NOT harmful to the hearing).
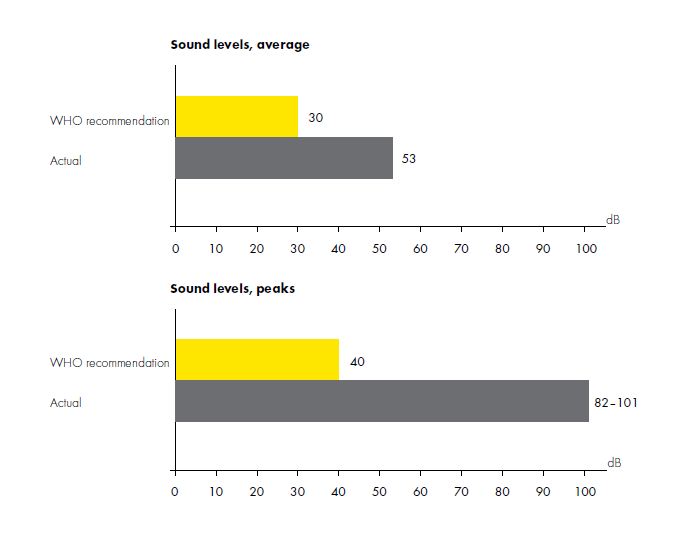
When it comes to the peaks in the investigated ICU – the numbers talk for themselves: the actual peak levels were from 82 – 101 dB – AND they exceeded 55 dB 68–79% of the time!
Patients’ reactions
Even though the numbers speak for themselves – the specialists chose to also investigate how the noise levels affected the patients. Interviews were made 2-35 days after ICU discharge and with 13 patients.
All of the interviewed patients shared rooms with one or two other patients and the space was divided only by thin fabric curtain which made it possible for speech to be heard from one bed to another.
The patients commented about the sounds coming from the patients beside them:
(patient no. 8):
’…but it was so annoying, this noise all the time, and I couldn’t sleep to escape the noise, it was impossible, it was so loud it was impossible’. [3]
Some of the patients also described the sounds as being experienced as scaring and frightening and they felt like having no possibility of shutting off the unwanted and unpredictable sound.
Acoustic intervention
The specialists group decided to include a room acoustic intervention to their project – to learn if this could have a positive effect on the ICU sound environment[4].

The intervention consisted of two two-bed ICU patient rooms (experimental and control) with different sound conditions (modified or not). The two rooms were laterally inversed but identical in size: height 2.70 m, floor area 29 m2, volume 77 m3. The walls were made of gypsum/concrete.

The acoustic intervention consisted of installing another ceiling only in the experimental room. The original ceiling was constructed of 13 mm. gypsum board with 20 mm. fibrous absorbent – and this was also what was in the control room. In the experimental room the ceiling was changed into an acoustic class A and hygienic ceiling.
Results
The study showed that it is possible to improve the sound environment in critical care – and it is possible to by just changing the room acoustic conditions (behavior, planning etc. were not part of the scope).
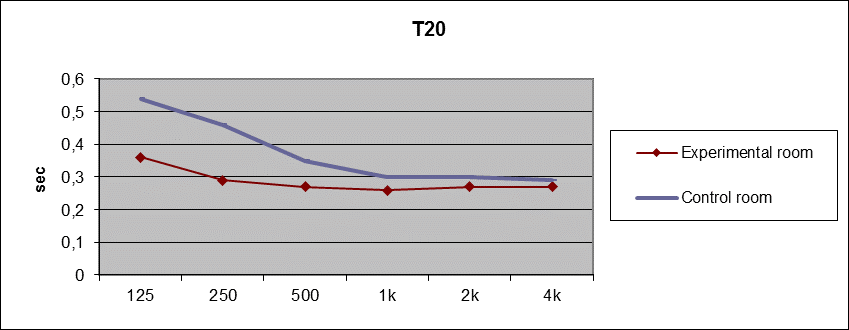
Room acoustic measurements were done and the group chose to investigate several acoustic descriptors. In building regulations around the world reverberation time (T20) is often the only descriptor to follow but speech clarity (C50) is crucial when it comes to critical care. Communication has to be clear at the same time as the sound does not build up – which is why speech clarity was included.
Values on reverberation time in both rooms met the Swedish Standard SS25268 that demands max. 0.5 seconds in ICU-rooms from 250 Hz – 4000 Hz (125 Hz is not included in the standard). Especially in the low frequency area the experimental room had improved and the curve was in general more uniform. On paper both rooms look ‘good’ when it comes to reverberation time, but the results on C50 showed another picture.
Speech clarity is of great importance and the measurements show that even when we have rooms with relatively short reverberation time – speech clarity can be bad. In the control room we see values under 5 dB in the lower frequencies which is highly problematic in a sound environment that has to support communication. Mid and high frequencies are considered to be OK in control room.
In the experimental room we see another world. Above 9 dB in all frequency bands is a great result – and this environment is even good enough to support speech communication for hearing impaired people[5]! Just noticeable difference according to ISO 3382-1 for C50 is 1 dB[6] so the perception of the two rooms are definitely different. The result for the experimental room is impressive in general.
Reverberation time is not enough
So what did the changes in reverberation time and speech clarity mean for the sound pressure levels in general?
Patients are affected by sound levels in hospitals – and during the years the sound levels has been increasing dramatically[7]. The reason for this can be a combination of more people in the buildings, more equipment, more complex tasks – and in general more sound sources. The hospital buildings on the other hand have not changed much – and the lacking of room acoustic treatment becomes a problem.
In this study there was a drop in sound pressure levels by approx. 3 dB in the experimental room in comparison to the control room. Knowing that the decibel scale is logarithmic 3 dB actually means that the sound pressure is halved, and the result therefor significantly important
On paper the control room met the Swedish standard – but despite this the patients didn’t find the sound environment supportive for sleep, communication or recovery in general.
_____________________________
[1] Nightingale F. Notes on Nursing: What It Is and What It Is Not. London: Gerald Duckworth Ltd 1859
[2]The specialists involved were primarily: Lotta Johansson, Institute of Health and Caring Sciences. Sahlgrenska Academy, University of Gothenburg; Ingegerd Bergbom, Occupational and Environmental Medicine, Sahlgrenska Academy, University of Gothenburg; Berit Lindahl, Borås University College, School of Health Sciences; Susanne Knutsson, Department of Nursing, School of Health Sciences, Jönköping Uiversity, Kerstin Persson Waye, Department of Occupational and Environmental Medicine, Sahlgrenska Academy, University of Gothenburg.
[3] Johansson L, et al: The sound environment in an ICU patient room – a content analyses of sound levels and patient experiences. Intensive and Critical Care Nursing (2012).
[4] Johansson L, et al: Evaluation of a sound environment intervention in an ICU: A feasibility study, Australian Critical Care
(2017)
[5] R. Plomp and A. J. Duquesnoy: Room acoustics for the hearing impaired, The Journal of the Acoustical Society of America 71, S19 (2005)
[6] ISO 3382-1:2009(en) Acoustics — Measurement of room acoustic parameters — Part 1: Performance spaces
[7] Busch-Vishniac et al., “Noise Levels in John Hopkins Hospital”, Journal of the Acoustical Society of America, Dec 2005, 118(6), p3629-3645
[8] See ref. 6