
When we are sick just opening the door to a hospital takes us out of our comfort zone. Our system is already stressed and our senses are therefore alert. We are more sensitive to sound and noise than normal – and in healthcare sound environments, this can be a challenge.
Sleep is essential
Patients are affected by sound levels in hospitals – and over the years, sound levels have been increasing dramatically[1]. The reason for this can be a combination of more people in the buildings, more equipment, more complex tasks – and in general more sound sources, but no matter what the sick body needs a calm environment to rest and recover. Sleep is essential.
European standards
A lot of research has discussed how sound levels in hospitals make it difficult for patients to rest and sleep and standards for room acoustics in patient rooms, examination rooms, and specialized areas are seen in many countries in Europe. Still, these acoustic standards are evaluating reverberation time only (except Finland which also takes STI into account[2]) and the big question is: are the standards good enough – and if not, how should we approach healthcare sound environments in the future?
Healthcare space
A hospital or healthcare space is like a small city that often works around the clock. Even outpatient clinics resemble offices with all types of rooms. We have ‘traditional’ smaller squared examination rooms where the doctors and nurses examine and talk to one patient (and maybe 1-2 relatives) at a time. We have open nurses’ stations and receptions in open-plan break-out areas where treatment takes place together with people waiting or communication between staff or staff and patients. We have patient rooms (1, 2, or more in one room) and staff offices, corridors, and waiting rooms. And we have specialized areas (ORs, NICUs, ICUs, etc.) where critical care involves a lot of staff members and specialized equipment – and where life and death tango on during day and night. Healthcare is complex!

Acoustic descriptors
It might be too optimistic to set demands on every room type in a hospital and one would have to invest a lot of time mapping down all activities in all room types also (e.g. not all patient rooms or corridors have the same activities) but on the other hand, to have one descriptor and one target value for a whole hospital is not sufficient either.
ISO 3382-3
In 2012, ISO 3382-3 was published. Like other standards, the method is intended for furnished rooms, and with no people present. The results can be used to evaluate room acoustical properties in open-plan offices and comparison to standards for healthcare, reverberation time is not included as such. Instead, background noise level, the sound power spectrum of normal speech, the spatial decay rate of speech (D2,S), A-weighted sound pressure level of speech at a distance of 4 m (Lp,A,S,4 m), distraction distance (rD) and privacy distance (rP) are included in the standard.
Hospital and open office – same same?
ISO 3382-3 concentrates a lot on speech and according to several studies patients and staff are disturbed by speech and communication – either if they can’t hear properly or if they hear too much!
In a study on the sound environment in an ICU patient room [3], a lot of patients reported conversations and speech (not directly relevant to them) as really negative regarding sleep and recovery. The patients in the study sometimes became involuntary listeners, and these dialogues made them both curious and frustrated – and sometimes afraid since they had to listen to stories without beginnings or ends:
‘‘Then sometimes when you lie there, half asleep. . .. the staff stand in the doorway and joking with each other, then I thought, are they talking about me or.?’’
Not only staff conversations in the corridor or at the nurses’ station are problematic generally, but sometimes conversations with neighboring patients can be just as problematic (you often can’t see your neighbor – but you can always hear them):
‘‘and then, once, he got so bad that a lot of surgeons came in, I don’t know how many there were, and they didn’t speak in low voices, they spoke loudly and a lot to each other about all these things and illnesses, (…). I put my fingers in my ears, I didn’t want to listen. Then I heard one of the surgeons say: but then we have to do a tracheotomy, then we have to do a tracheotomy (…).
Only sleep disruption because of speech?
It could be interesting to look into the descriptors from ISO 3382-3 and implement them (or some of them) in future standards for healthcare since a lot of healthcare space is complex with several sound sources and activities – just like the open office, and since research often conclude that speech can be problematic in healthcare it would be relevant. Some studies have already done that (read more about it in these blog posts about corridors, ORs, and different rooms in Copenhagen area hospitals)
But… when it comes to hospitals, the sound environment is even more complex and mechanical equipment and medical procedures also contribute to sleep disruption – and ‘medical equipment sounds’ are not part of ISO 3382-3.
Sleep disruption due to mechanical equipment
In a study[4] with 12 healthy subjects noises lasting 10 seconds were introduced during sleep stages N2, N3, and REM to evaluate their propensity to disturb sleep (learn more about sleep stages N1, N2, N3, and REM here). The clear results showed that electronic sounds were consistently more arousing than other sounds at the same noise dose. Still, staff conversations and voice paging were also found to be highly alerting, producing a 50% chance of arousal at 50 dB in N2 and REM sleep.
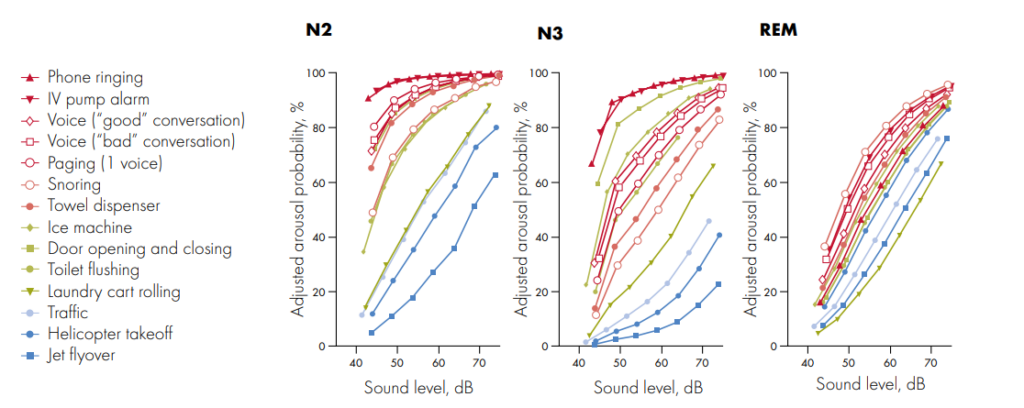
The probability of arousal to sounds presented in REM sleep varied less by sound type than when presented in N2 and N3 sleep but caused a greater and more sustained elevation of instantaneous heart rate. Even with the healthy subjects when their sleep was disrupted, even for a few seconds, their heart rates increased.
Speech, technical equipment, and …?
According to the two above-mentioned studies, both speech sounds and medical equipment sounds are problematic in healthcare. AND if we look at staff complaints they go in other directions (e.g. bad speech clarity and high noise levels contribute to errors[5]), so how should a healthcare standard take all this in consideration and what should it include?
Reverberation time is what we have in European standards today. And the descriptor IS highly relevant in some rooms. But it cannot stand alone. The descriptors in 3382-3 could be highly relevant in open healthcare environments where conversations are the main part of the sound sources. But how do we combine all this with the need for controlling the medical equipment? Could we maybe rethink and develop medical equipment that is not noisy? Or do we need the audible alarms and signaling devices to be part of the soundscape? For security reasons?
Is healthcare so complex that creating a fulfilling acoustic standard is mission impossible? Or should we dare to be ambitious and map down all the different rooms and activities (and possible sound sources) and set various demands to secure both patients’ sleep and recovery together with staff performance?
________________
- Read about a study where ISO 3382-3 was used to evaluate different office layouts. Find the reports and articles here.
- Read about acoustic standards and guidelines for healthcare here.
- Read about room acoustic descriptors (RT, C50, and room gain) here.
- Read about a workshop on open office acoustics here.
________________
References:
[1] Busch-Vishniac et al., “Noise Levels in John Hopkins Hospital”, Journal of the Acoustical Society of America, Dec 2005, 118(6), p3629-3645
[2] 796/2017 Decree of the Ministry of the Environment on the Acoustic Environment of Buildings (Finland)
[3] L. Johansson et al., The sound environment in an ICU patient room—–A content analysis of sound levels and patient experiences, Intensive and Critical Care Nursing, vol. 28, Issue 5, October 2012, Pages 269-279
[4] Buxton et al., Sleep disruption due to hospital noises, Ann. Intern. Med., 2012, vol. 157(3), p170-179
[5] Mahmood et al., “Nurses’ perception of how physical environment affects medication errors in acute care settings”, Applied Nursing Research, 2011, vol 24, issue 4, p229–237

