
In search of a noisy environment? Visit a hospital.
Studies show that noise levels are high due to operational activities, communication, alarms, and noise from medical equipment, along with structural sounds from the building (such as ventilation and closing doors).
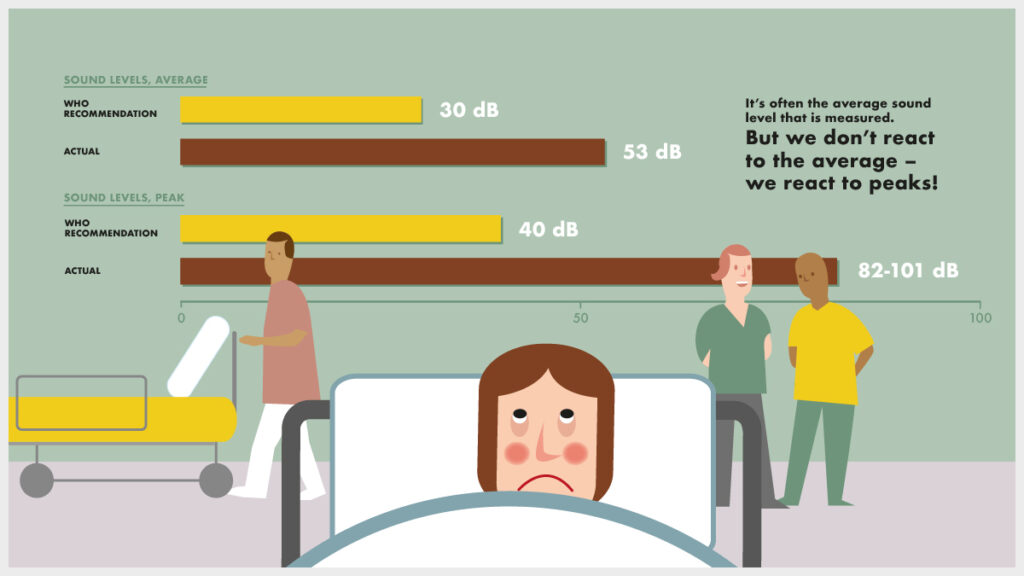
Already back in 1859, nurse Florence Nightingale declared how “unnecessary noise is the cruelest abuse of care which can be inflicted on either the sick or the well”. Imagine what her reaction would be today, with increasing noise levels in intensive care units and neonatal wards, that rarely comply with the WHO recommended noise levels. Arousals and awakenings are more or less expected.
What are the most annoying or intrusive noises in hospitals?
According to patients, disturbing sounds come in the form of conversations between staff, activity noise from the corridor (carts and footsteps in the hall), different alarms, medical equipment, the sound of doors slamming, and telephones ringing.
The list of the most annoying sounds according to staff in different hospital wards coincides to a great extent with the patients’ views. The two most disturbing sounds come from medical equipment and conversations between staff.
High on that list are also activity noises from the corridor (carts in the hall, footsteps in the hall), telephone calls, and different types of alarms. For a midwife or nurse in an obstetric ward, the most disturbing noise comes from screaming mothers giving birth (read about an acoustic intervention at the maternity ward at Randers Hospital, Denmark, here).
What can the noise lead to?
For patients, noise in hospitals has been suggested to increase the risk of cardiovascular response, pain, intensive care delirium, fragmented sleep, and reduced recuperation – even though other factors can also impact this outcome. Regarding sleep deprivation, research shows that up to roughly 40% of arousals and awakenings are caused by noise.
For staff, noise may cause annoyance, mental distraction, stress, and tiredness and lead to an increased risk for medical and caregiving errors, threatening patients’ safety. Research also shows that staff sometimes ignore, silence, or disable alarms. (Read about staff performance in different acoustic environments here).
What can be done?
While some sounds are unavoidable, many are totally or partially unnecessary.
We react to (disturbing) sounds already at a very low level. When sleeping, this means that it does not take much for our sleep to be disturbed. As a result, sound levels need to be reduced quite a lot to prevent arousal and awakenings.
Providing earplugs can of course help some, but this makes it more difficult to communicate, and the patient might feel enclosed. Studies have shown that more focus on visual and auditory stimuli can help. For example, a better sound environment can be reached by improving acoustics. (Read about the importance of good acoustics in a newly built hospital here).
No matter what, we should let Florence Nightingale’s wish to get rid of all unnecessary noise guide us – for the sake of both the sick and the well.
Some years ago, Kerstin Persson Waye presented this topic at the Care for Sound symposium. Watch the full presentation below. Kerstin Persson Waye’s research focus is to relate human response to sound characteristics.

