
Noise pollution
In recent years, several acoustic studies have noted that the sound environment in the Intensive Care Unit (ICU) is noisy and demanding. The noises are unpredictable and unexpected as they have numerous sources. The extent of the problem is not yet fully understood, but the impact of noise pollution in patient rooms in other hospital areas has been investigated.
Negative responses to noise
Cardiovascular responses, increased pain, prolonged stay, and sleep disturbances are some negative responses to noise. These effects must be taken seriously, especially in caring for the most seriously ill and vulnerable patients. One of the key roles of staff is to prevent and manage the environmental impact in the ICU; therefore, knowledge about sound and noise is fundamental and essential for all staff involved.
Research
A study conducted in 2012 measured and mapped the soundscape in 12 single-patient ICU rooms for 24 hours[1]. The overall mean sound level for the 24 hours was 53 dB (LAeq). The sound levels were without exception higher than the recommended level[2] and the LAF max levels exceed 55 dB 70—90% of the time. Maximum levels ranged from 82 to 101 dB (LAmax) and minimum levels were 31 to 47 dB (LAmin).
Patient experience
Most patients remembered some sounds from their stay in the ICU and whilst many were aware of the sounds they were not disturbed by them. However, some experienced feelings of fear related to sounds emanating from treatments and investigations of the patient beside them.
Where does the noise come from?
Park et al. conducted sound measurements for a total of 3 days in shared ICU rooms (2 patients)[3]. The findings support the observations of previous studies that ICU patients are exposed to a high level of noise, also suggesting that disturbing sound events may occur very frequently for a significant portion of time. It was also found that the staff-generated noise contributed most to the total acoustic energy and the number of perceived loudness peaks! This implies that noise issues in ICUs can be addressed, to a certain extent, by influencing the behavior or/and work routine of the staff members.
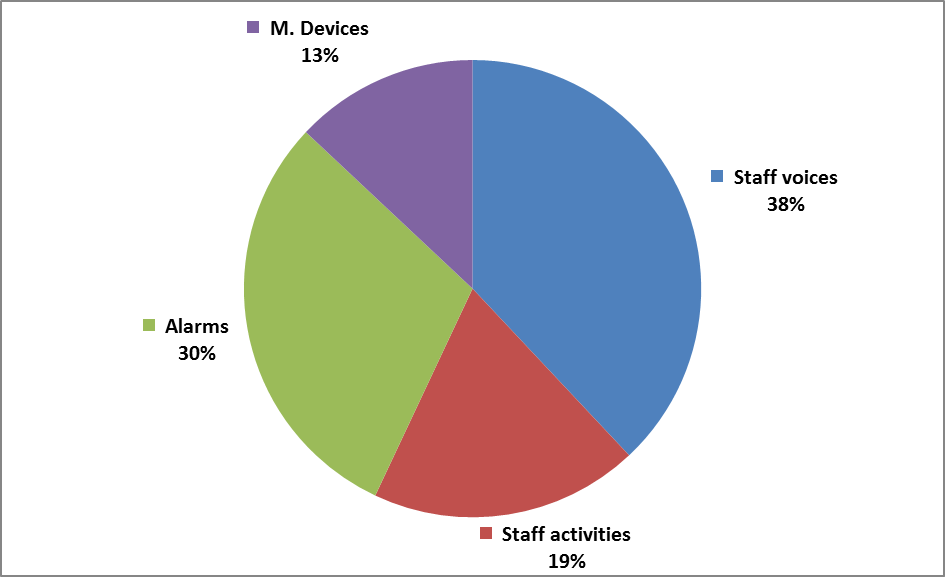
Staff members of the ICU spoke every ~15 seconds on average during the annotated 24 hours, carrying out 6 audible activities every ~6 seconds, while devices generated alarm sounds every ~15 seconds.
When interviewing patients after being treated in an ICU some findings need to be highlighted[4]. The meanings of being a patient in a sound-intensive environment were interpreted as never knowing what to expect next regarding noise, but also of being situated in the middle of an uncontrollable barrage of noise, unable to take cover or disappear.
The unpredictable shifts between silence and disturbing sounds stress the critically ill patient and impede sleep and recovery. The findings indicate the need to reduce disturbing and unexpected sounds and noise around critically ill patients in high-tech environments to facilitate well-being, sleep, and recovery. Nurses have a vital role in developing such an environment.
We can no longer claim that the patients are too critically ill to reflect on the surrounding sounds and noises.
The unpredictable shifts between silence and disturbing sounds do not create a healing environment for the critically ill patient but instead create stress.
Limited knowledge about the impact of noise
Further findings indicate that caring staff has a rather low theoretical knowledge concerning sound and noise in the ICU[5]. However, during interview sessions, they contributed with practical tips and ideas of how to create better sound conditions in the daily work but also described difficulties and barriers. These suggestions can be considered in the design of future interventions to reduce noise in the ICU as well as in other care settings. Take home message: We need to put the topic of sound and noise on the agenda for caring staff in the future!
Read another post about noise and the effect of room acoustics in the ICU here.
For more information about the topic contact Maria Quinn.
References:
[1] Johansson L. et al. The sound environment in an ICU patient room—–A content analysis of sound levels and patient experiences. Intensive Crit Care Nurs (2012).
[2] Berglund B., Lindvall T., Schwela DH: Guidelines for community noise. Protection of the human environment. World Health Organisation, 1999.
[3] Park et al. Source-specific analysis of the noise in an intensive care unit. Paper presented at Internoise Innsbruck, Austria, 2013, Sept 15-18.
[4] Johansson L., Bergbom I., Lindahl B. Meanings of Being Critically Ill in a Sound-Intensive ICU Patient Room – A Phenomenological Hermeneutical Study. Open Nurs J. 2012; 6: 108–116
[5] Johansson L. et al. Noise in the ICU patient room — Staff knowledge and clinical improvements. Intensive Crit Care Nurs (2016)

