
Acoustic interruptions
A recent study published in Critical Care Explorations revealed a potential relationship between acoustic interruptions and worsened perceived sleep quality. One of the results was that patients were exposed to 4,861 acoustic interruptions in total during the night! The conception that critically ill patients are too ill to reflect on their sound environment in the intensive care unit needs to be revised.
Background
Over the past 40 years, average noise levels in hospitals have increased by a full 15 decibels (dB) reaching levels of around 70 decibels, well above the World Health Organization’s recommended limit of 35 dB for a healing environment.
For patients, noise in hospitals has been suggested to increase the risk of cardiovascular response, pain, intensive care delirium, fragmented sleep, and reduced recuperation – even though other factors can also impact this outcome. Regarding sleep deprivation, research shows that up to roughly 40% of arousals and awakenings are caused by noise.
Scientific studies indicate that loud noise from equipment, alarms, and voices contribute to raising the patient’s level of stress and disrupt the healing sleep (Hsu, Ryherd, Ackerman, Persson Waye, ‘Noise Pollution in Hospitals: Impacts and Patients’, J. Clin. Out. Mgmt. 2012, vol. 19.).
Loud equipment noises, alarm sounds, and voices all disturb healing sleep and cause stress to patients. Patients in emergency departments, intensive care units (ICU) and operating theatres, and newborns in neonatal units, are especially sensitive to disturbing sounds.
New research published in 2021
Under the title ”Observations of Acoustic Interruptions Versus Ambient Sound Levels With Perceived Sleep Quality During Critical Illness” Alexandra K. Almberg et al have investigated how 14 patients ( – average 62 years old (53–66) and five were female) were affected by the sound environment in 2 days/nights in the ICU.
The researchers learned that there were 1,029 interruptions (≥ 20 dB increase over 1 second => 10 (± sd 15)) per patient per night and that four patients experienced at least 20 acoustic interruptions each from 22:00 to 05:00.
When monitoring acoustic interruptions ≥ 15 dB instead of ≥ 20 dB they found 4,861 interruptions in total meaning 48 (±49) times per patient per night. At this level, four individuals experienced greater than 120 interruptions.
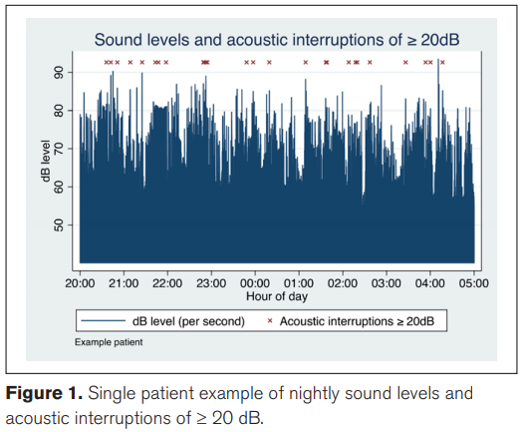
The study concluded a potential relationship between acoustic interruptions ≥ 20 dB above background and worsened perceived sleep quality based on interviews and monitoring of the patients.
We seem to forget how the sound environment contributes to recovery, medication intake, and infection risks. Patients, no matter if they have just gone through serious heart surgery or suffering from pneumonia need to recover quickly to avoid infections – and successful recovery is based on sleep.
Restorative periods of sleep
In 2015 a group of Danish researchers investigated the suitability of the sound environment in a modern intensive care unit (ICU) in promoting sleep by analyzing continuous audio recordings captured over three weeks (Ref: Lange et al: The sound of the intensive care unit – 3 weeks of continuous sound recording, 2015).
 They focused on restorative periods (RP). RP is defined as a period that starts after 5 minutes without disturbance of the sleep and the chocking data showed that the mean restorative period in 3 weeks was 6.2 minutes. Briefly, this means that you will get interrupted in your sleep 167 times in 24 hours because of a highly disruptive noise environment! The study also revealed that only one-third of the recorded days contained one or more RP ≥ 90 minutes. Knowing that the human sleep cycle is 90-110 minutes the study, therefore, concluded that an ICU patient rarely completed such a cycle.
They focused on restorative periods (RP). RP is defined as a period that starts after 5 minutes without disturbance of the sleep and the chocking data showed that the mean restorative period in 3 weeks was 6.2 minutes. Briefly, this means that you will get interrupted in your sleep 167 times in 24 hours because of a highly disruptive noise environment! The study also revealed that only one-third of the recorded days contained one or more RP ≥ 90 minutes. Knowing that the human sleep cycle is 90-110 minutes the study, therefore, concluded that an ICU patient rarely completed such a cycle.
Author: Mai-Britt Beldam, Market Development Manager at Ecophon.
________________________________
Read more about noise in the ICU here.
Read more about how to evaluate sound and acoustics in critical care here.

