
It was with great pleasure we visited this years Inter-Noise in beautiful Nantes in France. Nantes is especially know for being the birthplace of Jules Verne, master of adventure who was also a poet and one of France’s most prolific authors of all time, with a specific interest in science.
Some 1800 acousticians and researchers gathered from 62 countries to share research and network with eachother at the Cité des Congrès. The program was well structured with 117 session with a total of 1150 papers! Moreover there were 67 exhibitors showing the latest news of products and solutions applicable for this market.
This will summarise some of the healthcare-related presentations that took place in session 12.9. Acoustics of Hospital and Healthcare Spaces. Chaired by Pyoung-Jik Lee, and Elif Özcan.
Noise in an UK intensive care unit: a retrospective cohort study
T. HAMPTON¹, A. WAITE², A. TAHVILI² ¹ Liverpool School of Tropical Medicine|² University of Liverpool
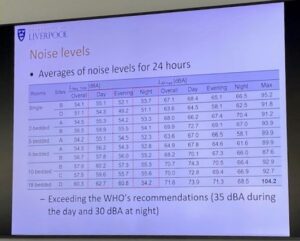
Excessive noise in hospital Intensive care units (ICU) has been associated with adverse health effects and human factor impacts acknowledged to negatively affect both patients and healthcare providers. The aim was to evaluate the acoustic environment of the Royal Liverpool University Hospital ICU versus WHO and UK guidelines. Noise measurements were taken from a six-bedded bay within the ICU between June and July 2022. This audit focused on noise data > 87dBA, acknowledging the national exposure limit established by UK Noise Regulations. A retrospective review of relevant patients’ records was conducted to identify potential noisy events during the audit period.
The results show the highest and lowest LAeq values were 77.9 and 63.5 dBA, respectively. All LAeq and LAmax noise measurements recorded exceeded the recommended guidelines. The noise fell below-recommended daytime guidelines less than 1% of the time. The top potential noise causes were patient repositioning/personal care, medication administration and suctioning.
The noise fell below-recommended daytime guidelines less than 1% of the time
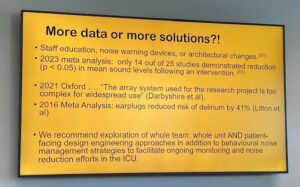
Thomas Hampton concludes that the noise levels in the old RLUH ICU considerably exceeed national and international guidelines. And that the findings highlight the need to address noise pollution in the ICU setting. Hospital staff and policymakers should consider implementing strategies and interventions for noise reduction in ICUs.
Quieter and calmer than before: sound level measurement and experience in the Intensive care unit at Erasmus Medical Center.
E. ÖZCAN¹, S. SPAGNOL², D. GOMMERS³. ¹ Critical Alarms Lab, Faculty of Industrial Design Engineering, Delft University of Technology |² Department of Architecture and Arts, Iuav University of Venice|³ Department of Adult ICU, Erasmus University Medical Center
Intensive care units (ICUs) are the ultimate socio-technological environments known for their loud sound levels. Alarms, noise produced by patient support devices, loud conversations, physical interactions with tools and the environment, in general, contribute collectively to a sound quality generally perceived as low. This paper reports the results from a study conducted inside the old and new ICUs at Erasmus Medical Center, Rotterdam, the Netherlands.
Sound level measurements have been collected continuously for three weeks in several matching rooms inside the old and new ICUs at full operational levels at a one-year distance from one another. The results support the idea that changes in architectural layout, procedures, and culture have contributed to a significant decrease in the measured sound levels across all daily shifts, both inside patient rooms and in the nurse stations.
The comparison of sound level measurements indicates that the new hospital is significantly quieter than the old hospital, both in nurse stations and patient rooms. Nurse stations measure on average 9–10 dB less on the daily peaks (i.e., shift changes) and 10–12 dB less at lunch and dinner times; patient rooms measure 3–4 dB less overall and nurse visits every two hours are significantly less pronounced in the measurements. The corridors showed no significant change.
The expert interviews identified three main topics that contributed to the reduction in sound levels: new architecture (layout and fittings), introduction of new medical devices, and change in team dynamics.
Nurse stations measure on average 9–10 dB less on the daily peaks
Our review of the future needs for sound measurement tools revealed that for effective noise mitigation, contextual sound source detection is required for two reasons. First, the conditions in which sound events occur need to be clear to determine the psychological effect of sound events. Secondly, to prevent unwanted sounds on the work floor through behaviour change. Healthcare professionals need actionable information regarding the appropriateness of the sound to the context.
Therefore, we propose that to introduce sound-driven solutions that are listener-centric and positively affect the acoustic environment (sound reduction or sound quality improvement), we need to gain insights into how sound and sound-producing events in a functional environment affect healthcare professionals and their workflows. Reducing sound is not limited to noise mitigation in sound-producing electronic products, it is a collective effort with behaviour change required of the healthcare professionals as much as a corporate effort to purchase quieter equipment, introduce less noisy caregiving protocols, and possibly change the architecture.
The impact of noise in intensive care units on the wellbeing of healthcare workers
P.J. LEE¹, Z. SONG¹ ¹ University of Liverpool
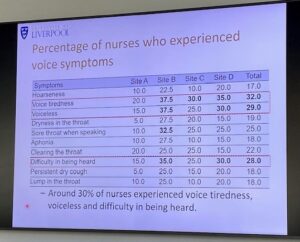
This study investigates the impacts of noise in intensive care units (ICUs) on the well-being of healthcare workers. To achieve this, a series of research activities were conducted. Firstly, noise monitoring was carried out at ICUs in China to explore the noise levels and sources. Secondly, a questionnaire survey was performed with ICU nurses to investigate the risk of voice disorders, utilizing the Voice Handicap Index (VHI-30).
Additionally, the voice use of ICU nurses was monitored using a wearable microphone. Thirdly, the hearing of ICU nurses was assessed through the Pure Tone Audiometry test (PTA) and Digits-In-Noise (DIN) test. Lastly, semi-structured interviews were conducted to explore how ICU nurses perceive and react to the noise in ICUs.
All measured noise levels in the ICU patients’ rooms in four Chinese hospitals exceeded the WHO guideline by at least 20 dB. Talking/voices inside the wards were most frequently heard, followed by footsteps, door-closing, and general activities. These findings emphasise the potential impact of prolonged and intense work schedules, particularly in noisy environments like ICUs, on the verbal communication quality, vocal health, and hearing health of nurses. The most frequently reported symptoms from both countries were ‘voice tiredness’ (20.5%) and ‘clearing the throat’ (18.3%).
Optimization of speech intelligibility in street-facing rooms of adult care home based on acoustic simulation
Zhengnan Xiang, Zhixiao Deng, Faculty of Architecture and City Planning, Kunming University of Science and Technology, Kunming, Yunnan, 650500, China
Due to the limited availability of urban land in China, many adult care facilities have resorted to constructing roadside living spaces. However, this has led to a significant issue of traffic noise disturbance. Besides, many rooms lack control over indoor reverberation. As a result, the communication efficiency of the residents might be greatly impacted. This study investigates the impact of traffic noise level, room size, and surface sound absorption on speech transmission index (STI), based on a typical room layout and conducted using acoustic simulation.
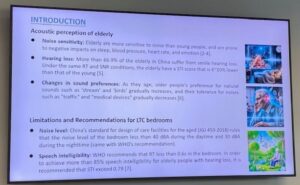
Previous research has demonstrated that elderly individuals are particularly susceptible to the adverse effects of traffic noise. Symptoms such as irritability, nervousness, memory impairment, and insomnia are more likely to be exhibited by them under its interference. Compared to younger individuals, the elderly have a higher sensitivity to noise stimulation, rendering them more susceptible to its negative impacts on sleep quality, blood pressure, and heart rate.
The simulation results indicated that to achieve the required STI over 0.79 for elderly residents, it is imperative to control the road noise interference below 40 dBA and ensure that the room reverberation time (RT) is under 0.42 s. To achieve this, it is recommended that for a road with a noise emission level of 72 dBA, the distance between the roadside room and the road should not be less than 10 m. Additionally, windows with Rw+Ctr over 28 dB without road sound barriers (over 20 dB with sound barriers) should be installed.
Besides, the room area needs to be controlled within 20 m2 and an acoustic ceiling with NRC>0.65 should be installed. When an acoustic ceiling with a noise reduction coefficient (NRC) exceeding 0.65 is installed, both RT and STI levels in typical rooms are significantly enhanced. This improvement is particularly noteworthy in larger double occupancy rooms measuring 30 m2, where the RT value can be maintained below 0.6 s. However, to simultaneously attain an STI value of at least 0.79, it is necessary to limit the room area to within 20 m2.
—————————————————————————————————————————————————————————————————————————————————————
This year’s Healthcare acoustic session was very impressive and contained more than the above-mentioned presentations. Thanks to all the presenters for their important and interesting work. And the session chairs who made this program available and hosted a nice interactive session!
More reading on Healthcare acoustics at previous Inter-Noise:

