
Standards in Europe
Standards and guidelines for room acoustics in healthcare are lacking in general and very few countries have mandatory regulations in this field. And even in countries with guidelines for other public buildings (e.g. schools) healthcare standards – and particularly detailed standards including corridors don’t exist. Just to mention a few – Czech rep. and the Netherlands are still to develop any kind of local standard for hospital corridors.
In Spain it is a bit tricky since the guideline CTE DB HR states that ‘common areas’ should have sufficient sound absorption such that the equivalent sound absorption area, A, is at least 0.2 m2 for each cubic meter of the volume of the enclosure.
‘Common area’ is defined as areas giving service to several ‘units of use’ – and ‘units of use’ is a building or part of a building that is intended for a specific use, and whose users are linked to each other, either by belonging to the same family unit, company, corporation or by being part of a group or collective that performs the same activity. And this could be a hospital corridor!

In countries where we have had local guidelines/standards for healthcare for many years, the demands for corridors often meet the same target values as examination/treatment rooms; e.g. Denmark[1] where the target value is 0.6 sec. for T20 – or in the UK[2] where the target values are related to absorption.
In the UK the requirement is for a minimum area of absorption equivalent to a Class C-absorber, covering an area at least equivalent to 80% of the floor area. If materials of a better absorption class (Class A) are used the required minimum surface area will be reduced.

In comparison, the French[3] regulations are related to ‘all’ public corridors (not only in hospitals) and the demands are stated as the equivalent of 1/3 of the floor surface as a quantity of absorbing material.
In Norway[4] the demands for corridors are to be found in the paragraph for ‘public areas’ and recommends a maximum reverberation time based on room height x 0,2.
In Finland, the standard SFS 5907 looks a bit different and classifies buildings into A, B and C with different target values for reverberation time: 0.6 s for class A and B buildings and 0.8 s for class C buildings. These numbers are also related to corridors.
But what is a corridor after all? What is its function of it?
The DIN standard in Germany[5] states recommendations for hospital corridors with a “quality of stay”, such as waiting areas highlighting the minimum ratio between the surface area of absorption/room volume and divided into height <2.5m or >2.5m.
But is a corridor always ‘just’ a path from A to B including waiting areas – or do corridors more and more look like open spaces like corridors/break-out spaces in schools where kids also go to work in groups?
The traffic corridor

All hospitals have corridors ‘just’ for traffic. Corridors where the function is to make logistics happen at all times. Yes – conversations take place but the overall function is the transport of people, equipment, or both. Acoustically these corridors are not as hard to handle as more ‘’complex’’ corridors – often it is enough to focus on low sound pressure levels and sound propagation.
The ward corridor
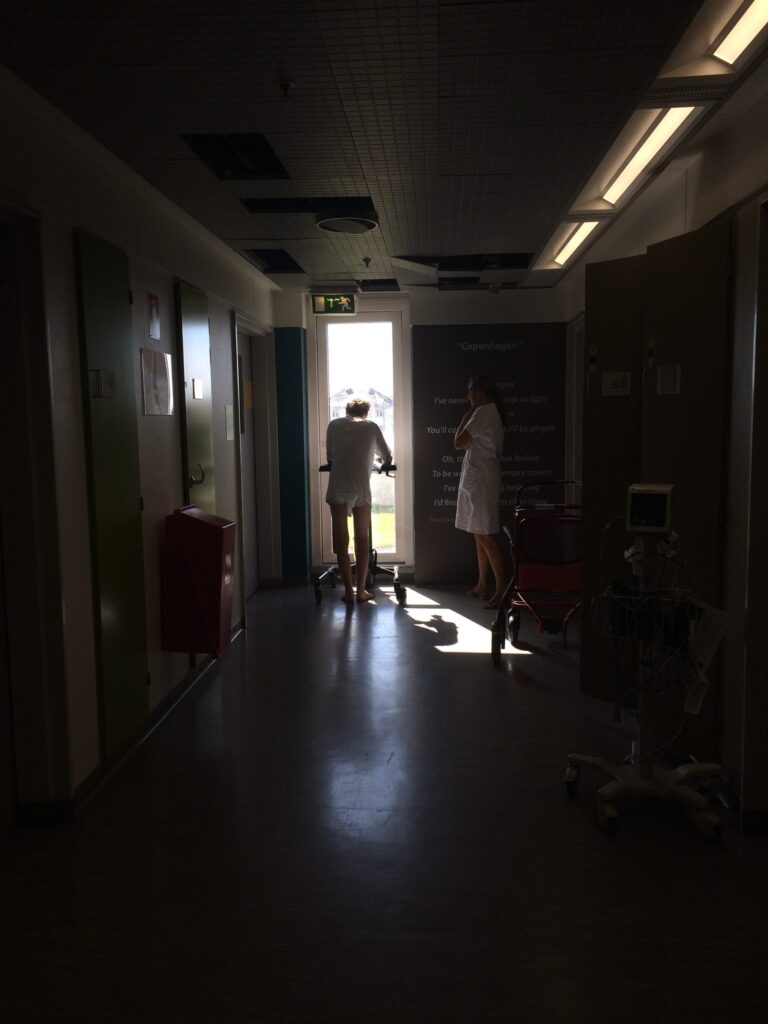
Corridors in wards used to be a path from A to B where staff members went from one patient room to another, where patients were moved (in their beds) pre- and post-operation – or where people would sit and wait in silence. Today it is very often that both treatment, examination, and communication happen in the same space.
Visually you are not shielded very often and when it comes to the sound environment these corridors can be very noisy. Now and then, patient wards are lacking space for the patients in the patient rooms so it is not impossible also to see patients in their beds trying to recover IN the corridor. Also, it is often that recovery treatment/exercise happens in these corridors.
Nurses’ prospective memory is affected
When it comes to acoustics these corridors should have more attention. A recently defended PhD-study (read more about it here) revealed that nurses are highly affected by sound and noise when it comes to prospective memory and a lot of their work happens in the corridor.
An insufficient sound environment will cause mistakes and in the long run, the lack of privacy, comfort, and tranquility will hurt both patients and staff. Keep in mind that hospitals work around the clock and corridors are likely to be busiest day and night.
The Sandwell Case
At Sandwell General Hospital in Birmingham, England, replacing the old, reflective ceiling with a highly sound-absorbent Class A ceiling reduced noise levels in the corridors of Priory Ward 4 by half. Before the refurbishment, it was quite a noisy environment, since all the surfaces were smooth with hard finishes.
Owing to the constraints of testing in a working hospital environment, ceiling changes were allowed only in the corridor area. Yet this action alone produced a significant improvement in the acoustics in both the corridor and the ward and it was seen that several acoustic descriptors were relevant to evaluate.
Sound propagation and privacy
When it comes to the corridor as such it was particularly interesting to look at sound propagation and privacy since reverberation time does not say much about if you are bothered by sound and noise that is not relevant to you. Also, it was important to secure that confidential conversations didn’t ‘travel’ too far down the corridor, and finally it was crucial to secure as low sound pressure levels as possible.
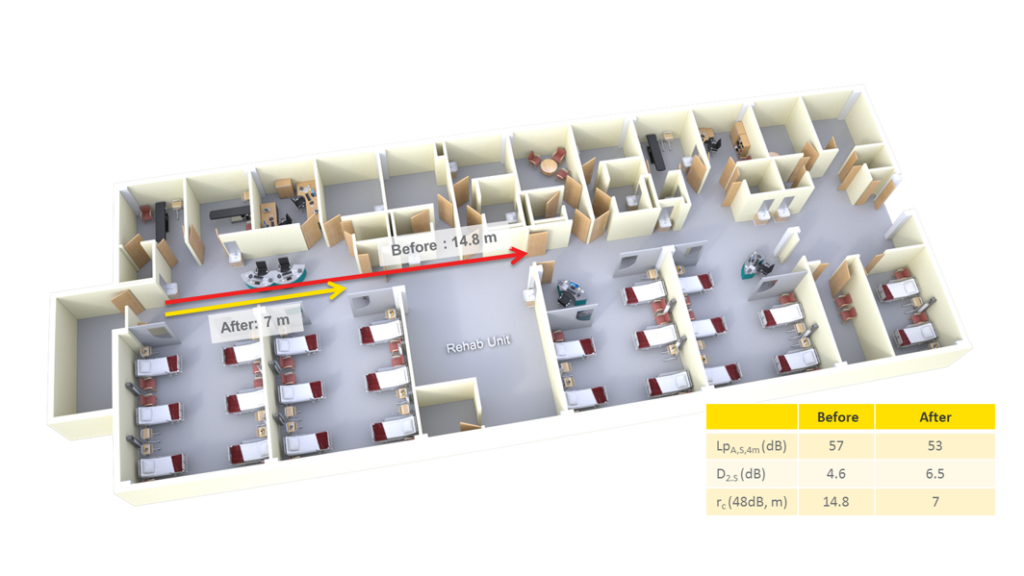
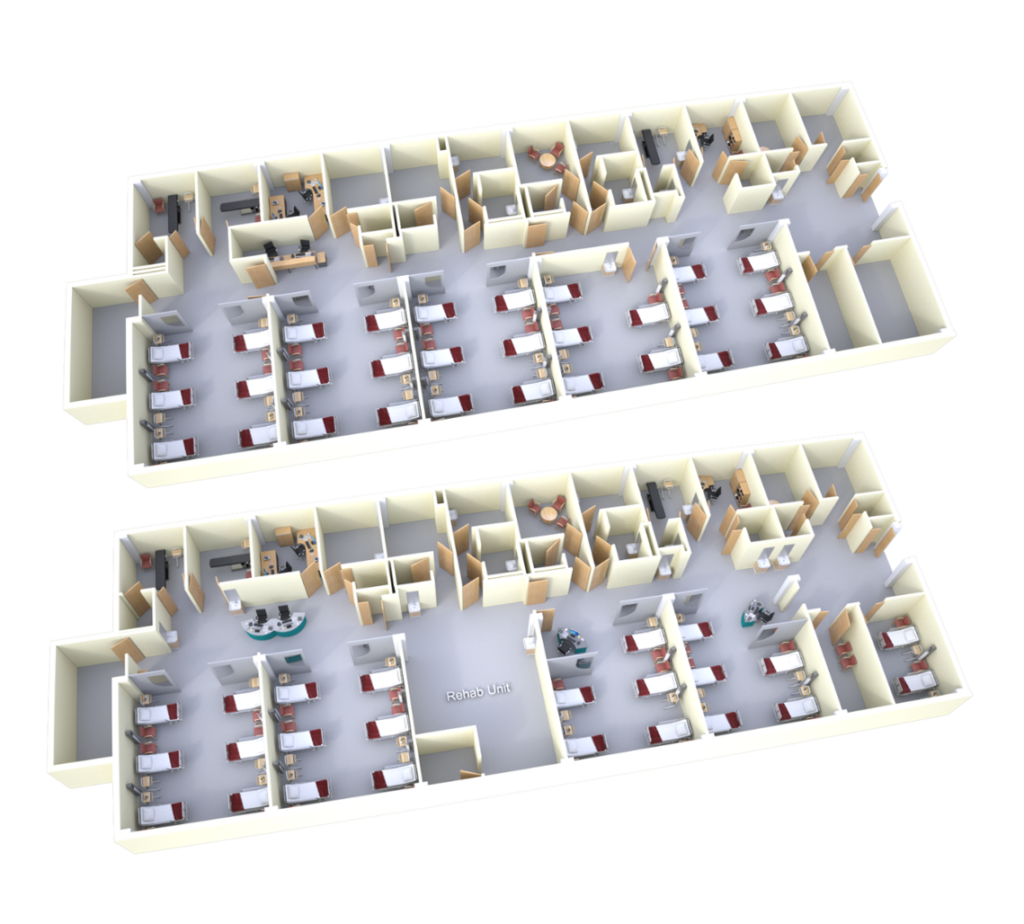
RT, C50/D50, and STI
Since the layout of the ward was slightly changed (more open + nurses’ stations were changed – one primary station in the corridor, smaller ones in patient rooms) it was also relevant to look at room acoustic descriptors in these areas knowing that a lot of conversations would take place here. Also at the primary nurse’s station, it had been possible to lower RT and make speech clarity, definition, and STI better at the same time as the sound propagation was controlled.

There is no doubt that the Sandwell case reveals the need for focusing a lot more on the acoustic design than ‘just’ to reach a target value for RT or absorption area. Today, corridors are more or less like outbreak spaces in schools and here you would never doubt if several acoustic descriptors were relevant.
Corridors in outpatient areas
These corridors are really busy and everything can happen during the daytime. In comparison to the ward, patients don’t stay during the night but treatment, examination and communication happen. Often there is also a reception in this corridor and besides the patients, relatives often contribute to more sound sources.
The patients don’t require acute treatment yet still they can feel very bad and therefore the sound environment will affect them highly. When you are sick you are vulnerable to sound and high sound levels and peaks will stress your system further.

Staff working in an outpatient clinic are seeing a lot of different patients during the day. And the constant traffic of people, treatment and examination can be very noisy if the corridor is not prioritized acoustically.
You can rarely shield yourself because the next patient is already waiting for your attention. Also, keep in mind that patients and relatives sometimes get not-so-good answers in these facilities which also adds an extra stressor to the system.
Imagine being a parent to a child with cancer waiting in the noisy corridor to get to see the doctor – who will tell you if the chemotherapy worked or not…
[1] BR20 – the Danish Building Regulation
[2] HTM 08:01 – Health sector buildings: acoustic design requirements
[3] Arrêté du 25 avril 2003 pour les établissements de santé
[4] NS 8175 – Lydklasser for bygningstyper
[5] DIN 18041:2016-03 – Raumgruppe B3 “Räume zum längerfristigen Verweilen”.

