
Noise levels – how it is experienced by staff
We have building regulations for room acoustics in hospitals in Intensive Care Units (ICU). But are they enough to create a good environment for both staff and patients? Recently a new study from Copenhagen hospitals was finalized so let’s take a look at some of the findings.
Master thesis student Hannah C. W. Jakobsen at DTU, Department of Civil Engineering, explored the sound environment in three ICUs and one neurological unit with both acoustic measurements and surveys.
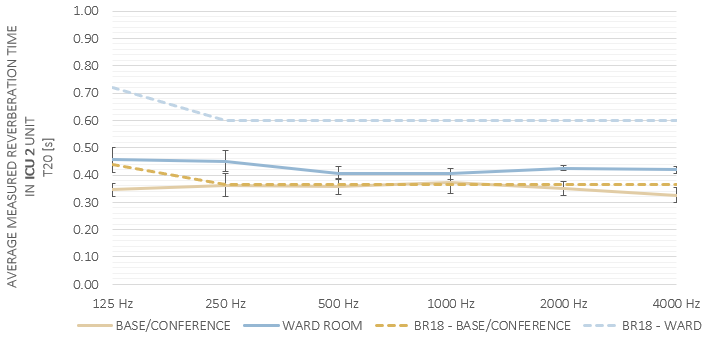
Reverberation times comply
It was found that the measured reverberation times (RT) in the wards generally met the requirements stated in the Danish Building regulations (BR18) [1]. BR18 commands a maximum RT value of 0.6 seconds and it allows a 20 % exceeding at 125 Hz.
Also, the calculated speech intelligibility was very satisfying. However, the perceived speech intelligibility expressed by staff was poor! This was in part attributed to the high noise levels in the units. Speech intelligibility expressed as Speech Transmission Index (STI) was above 0,7 and in some rooms around 0,8.
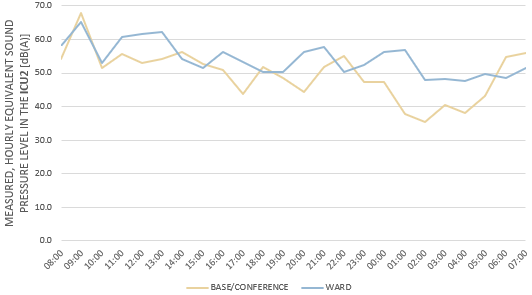
None of the patient rooms met the recommended thresholds for noise as directed by the World Health Organisation [2]. Staff feedback showed noise to have a significant negative impact on the ability to concentrate, and increase the feeling of stress.
From the questionnaires about half of the staff respondents in all units expressed being disturbed by noise to some extent or even very disturbed.
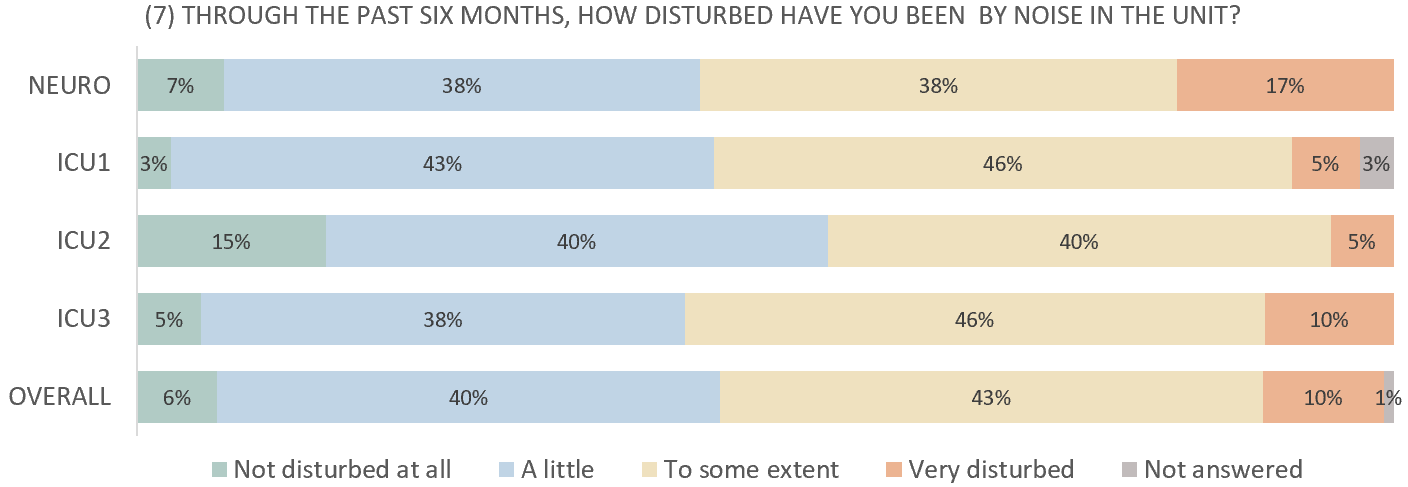
The fact that this is an issue experienced by a large part of staff members in all units – speaks to a general problem!
half of the staff respondents were disturbed by noise to some extent, or even very disturbed
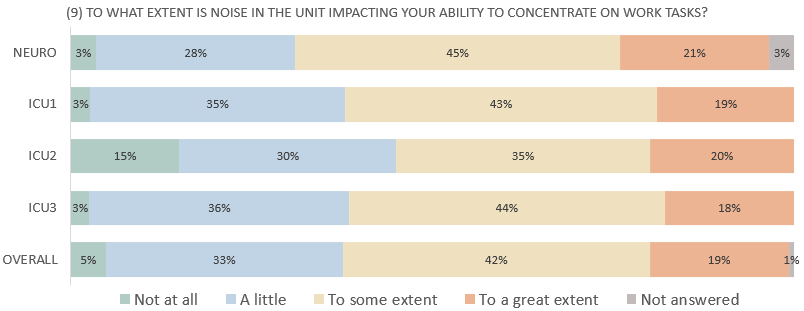
In all four units, upwards of 20% of the staff also expressed that their ability to concentrate is greatly affected by noise.
Measurements and questionnaires
We will only look closer at one of the rooms from the study, ICU2. ICU2 is the unit located in the newest facilities compared to the other units in the project and it was taken into use in the fall of 2020. Like the other ICUs, the patient group is critically ill, and all medical staff is specially trained. Critically ill patients with severe head traumas, who need specialized care, come from all parts of the Danish Commonwealth. At times, the flow and work pressure can be very hectic, and patients are admitted and reassigned to other units depending on urgency and capacity.
Like in many ICUs, the 24h observational function applies in ICU2. The workstation of the observational nurse is located inside the ward, meaning the office space of the nurse is at a desk in the corner of the patient’s bedroom.
ICU 2
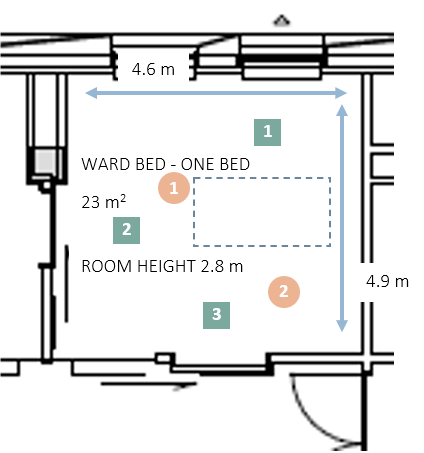
The room is a standard single bedroom with a room height of 2.8 meters. Acoustic measurements (RT, SPL, STI, D50) were conducted and the orange circles indicate source positions: while the green squares indicate the receiver positions. The perceived sound environment by staff is evaluated through questionnaires. The questionnaire aims to investigate if current conditions are sufficient to create satisfying sound environments for a workplace and a place of healing.
ICU2 room:
In ICU2, the pressure in the patient’s brain is constantly monitored, and noise can increase the pressure. For prevention, staff sometimes use hearing protection on sensitive patients. LAeq, night in the ICU2 ward is disturbingly high. To the patient, it is comparable to trying to sleep in a busy restaurant. High noise levels also affect the staff´s ability to concentrate and work during the night.
The fact that ICU2 shows the highest equivalent sound pressure levels and LA, max despite being the newest unit and having single-bed ward rooms is alarming. It can indicate that staff having their workstation in the room contributes negatively to the sound environment in the wards.
Results and findings
A slight decrease in the hourly equivalent sound pressure is seen during night hours. But the general sound level is significantly higher than the recommendations of WHO. Some of the findings behind these high levels.
-nutrition and fluids through intubating, noisy and often occurring
-many functions located in the same space
-hectic environment, too busy to take actual breaks. Personal conversations, that would usually belong in a break room move to the observation rooms
– conversations propagate and disturb other staff trying to concentrate on work tasks
– noise emitted by med-tech equipment, at times so loud it overshadows alarms
– difficult for nurses to concentrate, which is necessary to ensure the medicine and dosages are correct
A way forward
This study shows the inadequacy of current regulations and building traditions but also points out valuable tools to use in future design.
- Use questionnaires and let staff highlight problematic areas and sources of noise in their work environment.
- Combine this with observations and noise measurements, and gain a holistic overview to improve the noise in the ICU.
- Identify areas of improvement with a broader perspective than only acoustic parameters, and a more nuanced insight can be achieved and serve as a tool for improvement.
Want to know more on room acoustics in hospitals – see this post on sleep in the ICU and how to evaluate sound and acoustics in critical care!
[1] Bygningsreglementet, “Bygningsreglementet, br18, tekniske bestemmelser krav 17, lydforhold,” 2018.
[2] B. Berglund, T. Lindvall, and D. H. Schwela, Guidelines for community noise. World Health Organization, 1999.

