
It is no secret that the effect of sound in healthcare can unfluence people negatively. Various studies over the years have shed light on how care and cure of patients get difficult if the sound environments are not supporting the activities.
Patients suffer
Patients are affected by sound levels in hospitals – and over the years the sound levels have been increasing dramatically[1]. The reason for this can be a combination of more people in the buildings, more equipment, more complex tasks – and in general more sound sources.
High sound levels in healthcare facilities are known to: impair sleep, increase stress, delay post-illness rehabilitation, aggravate agitation, cause psychiatric symptoms, escalate restlessness, increase respiratory rates and increase heart rates[2].
But what about the staff? They are ‘just having another day at the office’ – how are they affected by the sound environment?
Prospective memory
Jikke Reinten recently defended her Ph.D. with the title: ”Exploring the effect of the sound environment on nurses’ task performance – An applied approach focusing on prospective memory”. And her findings clearly show that staff (in this case nurses) are affected by the sound environments they work in.
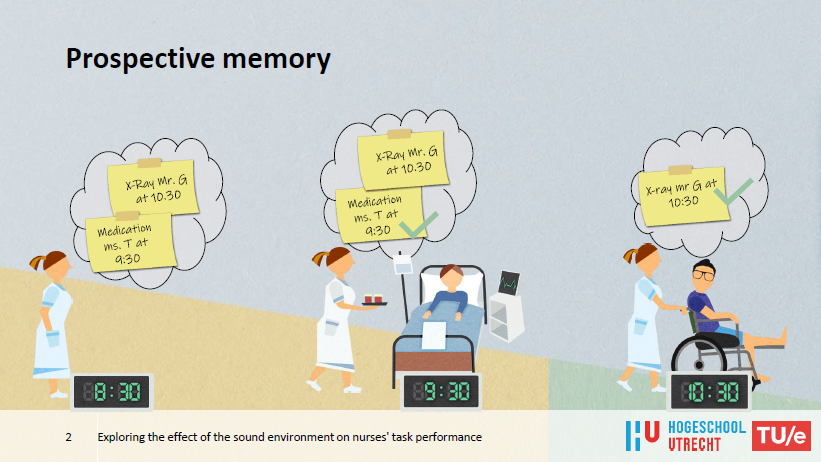
Dr. Reinten’s work concentrates on the prospective memory (PM) of nurses and she describes how an important aspect of a nurse’s job is to carry out intended care activities at the right time. This requires prospective memory. Examples of typical PM tasks in the context of nursing are remembering to administer medication at a specific time or turning a patient in every hour.
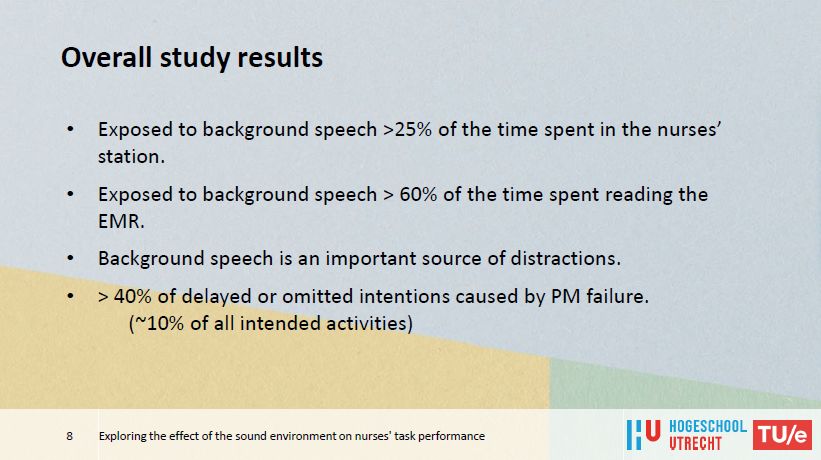
The investigations revealed that prospective memory failures were the cause of over 40% of the care left undone.
Different sound conditions
In her study, she analyzed the sound conditions a nurse was exposed to during a day shift and simultaneously investigated the activities that took place. Some of the findings in the study showed that for a large percentage of their time, nurses were exposed to intelligible background speech while performing the important task of forming prospective memory intentions. It was also seen that the nurses were often disrupted or distracted due to background speech.
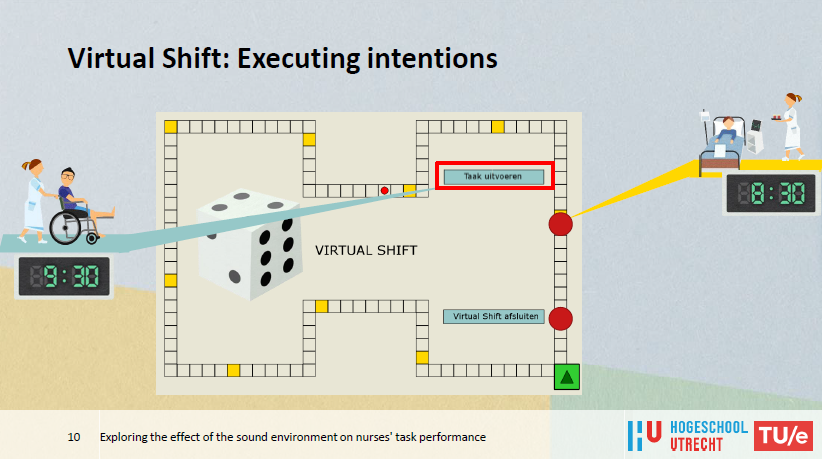
Because of these findings, Dr. Reinten decided to do an experimental study on the effect of intelligible background speech on the forming and retrieving of prospective memory intentions. The experiment fell into two parts:
- Forming intentions while reading electronic medical records.
- Retrieving intentions during a ‘virtual shift’ in the form of a board game.
To measure the effect of sound conditions on nurses’ tasks performance, room acoustic modeling software was used to simulate three realistic acoustic environments (clear speech in a room with an acoustic treatment – short reverberation time, unclear speech in a room with little acoustic absorption – long reverberation time, no speech – no disruption).
The overall results were as follows:
- Best performance: no background speech.
- Worst performance: background speech in a sound-absorbing room causing a higher speech intelligibility.
- Highest perceived disturbance: background speech in a reverberant room causing higher sound levels.
Next steps
We had the opportunity to discuss with Dr. Reinten after her defense – and we were curious about what her advice for hospital layout in the future would be.
One of the main issues today is that nurses cannot shield themselves when doing brain work and the behavior of colleagues (just being nice and friendly) is therefore a challenge. Dr. Reinten commented that talk and conversations around a nurse doing an important task are disruptive even if the nurse doesn’t directly take part in the conversation. A ‘halation’ where you pick up bits and pieces of the content can cause the next mistake. Also, sometimes the nurse doing the important task NEED the information that is given – but the timing can be problematic.
Activity-based acoustic design
Dr. Reinten explains that corridors in hospitals are today complex ‘rooms’ where a lot of distractions take place. And it could be relevant to work with a corridor layout where it is possible for the nurses to shield themselves – just for a few minutes (visually and acoustically). It could be interesting to see if ‘office pods’ / ‘phone booths’ or something similar could make a change in this matter.
If we could separate concentration and communication in a nurse’s workday, maybe this would have a positive effect on prospective memory.
For an efficient and safe hospital in general, activity-based (acoustic) design should be prioritized!
Remember comfort!
Dr. Reinten mentions that one thing that should not be neglected is the importance of COMFORT for the staff. Her study ‘only’ concentrates on a small part of how sound affects staff and she states that comfort is more important than we may know. If it is neglected – it affects staff long-term and will maybe cause more trouble than challenged prospective memory. Yes – nurses are interrupted by intelligible speech but if hospitals are too noisy because of lack of acoustic treatment, the staff will be affected negatively – so we have to design for the different activities that take place and for the different people in the facilities.
NB. All pictures/graphics in this article are taken from the presentation that Dr. Reinten did at her Ph.D. defense.
_____________________________
[1] Busch-Vishniac et al., “Noise Levels in John Hopkins Hospital”, Journal of the Acoustical Society of America, Dec 2005, 118(6), p3629-3645
[2] Weise, “Investigation of patient perception of hospital noise and sound level measurements: before, during and after renovations of a hospital wing”, Architectural engineering – Dissertations and Student Research, 2010, Paper 4, p7

