Healthcare and sound
Some of us have tried to be sick in a hospital – most of us have tried to be relatives to a sick person in a hospital – and all of us have been affected by sound. Sometimes we are aware of it – sometimes we suffer without knowing it.
This following study from Karolinska University Hospital shows us how patients in different acoustic conditions are affected differently. And it tells us that when we build healthcare facilities we need to think about good room acoustics and low sound pressure levels.
A total of 94 patients admitted to the intensive coronary heart unit at Karolinska University Hospital for evaluation of chest pain were included in the study. Patient groups were recruited during bad and good acoustics, respectively[1].
The room acoustic conditions
The physical environment was manipulated in two steps. First the original ceiling was converted into a grid system with 13 mm. plaster board tiles – corresponded to class C. The second step was to change the ceiling tiles – from the plasterboard to a 40 mm. glasswool acoustic tile that was also fulfilling the hygiene demands. This solution corresponded to class A. Both assessment periods lasted for 4 weeks.
The results
Patient rooms – from 0.9 to 0.4 sec. (T20)
Acoustic measurements were done in both conditions and the results showed that going from bad to good acoustics made the sound pressure level drop 5-6 dB in the patient rooms at the same time as the reverberation time dropped from 0.9 sec. to 0.4 sec. Speech transmission index was also measured and it went from 0.64 to 0.86 in the patient rooms.
The people
‘Accordingly, the staff felt fewer demands and less irritation during the good acoustics period’ – this is a statement that it hard to measure in numbers – but it tells us a lot!
Higher heart rate
The study also showed that the patients who were sickest – were more vulnerable to sound and bad acoustics than the patients that were not in the same vulnerable condition – the heart rate of the sickest was more affected:
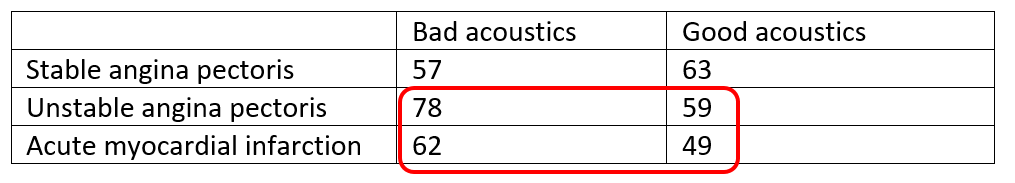
Another striking result was also that there was a higher incidence of rehospitalizations at both 1 and 3 months in the group of bad acoustics compared to that in good acoustics. Furthermore, patients in the good acoustics period found the staff attitude to be much better than during the period of bad acoustics.
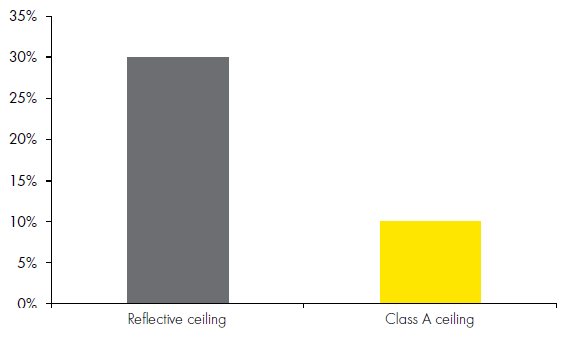
More medication
Finally, the medication intake in the two room acoustics conditions were different. Nearly all the patients were on peroral beta-blockers[2], and extra intravenous treatment was given mostly on the indication of pain. There was a significantly higher frequency for the need of extra intravenous beta-blockers in the group during bad acoustics.
Reseach since many years have showed the need for good room acoustics in healthcare facilities – and we need to work for better acosutic standards all over the world to secure this (read another post about the topic here). The facts talk for themselves: Patients suffer – they cannot rest or recover in noise and bad acoustic conditions.
A research summary guide about acoustics and sound in healthcare facilities can be found here.
__________________________________
[1] Hagerman et al: Influence of intensive coronary care acoustics on the quality of care and physiological state of patients, International Journal of Cardiology, Volume 98, Issue 2, 15 February 2005, Pages 267-270
[2] Peroral beta-blockers = ’normal’ heart medicine


