
Introduction
Speech in the ICU affected
Intensive care units (ICU) can be noisy and disruptive environments from both a patient recovery and workplace perspective, affecting speech intelligibility. Noise and poor ward acoustics have been linked to sleep disturbance and protracted recovery times in patients, as well as increasing workplace stress, fatigue and occupational burnout in healthcare professionals [1].
Given that noisy environments are detrimental to speech intelligibility (SI), this could lead to a higher incidence of mistakes [2] and miscommunication between nurses and patients. Therefore, jeopardises the health and well-being of patients and degrades the quality of care that can be provided.
However, ICUs are also places in which personal and confidential information is often shared. In which case, the content of speech should not be so intelligible to maintain privacy and minimise disturbance.
Investigation of speech and privacy
This study investigated speech intelligibility (SI) and Privacy conditions in ICU environments.
To investigate these spaces, a number of ISO 3382-2 & 3 parameters were measured to reflect that those spaces share characteristics of both ordinary household rooms and open-plan office work spaces, with separate beds representing partitioned work spaces.
The acoustic design criteria and building regulations concerning ICUs are generalised and not particularly detailed. For example, the Danish Building regulations (BR18) simply specify a reverberation time of 0.6 s. Investigating a broader comprehensive set of metrics, such as STI and Clarity, would help in defining these spaces for speech conditions, communication and privacy.
Further to the limited design criteria, the furnishing and acoustic treatment that is applied to ICUs is often limited in use due to hygiene concerns in sanitising surfaces. Furthermore, curtains and partitions between beds are frequently used with little consideration for their effect on the acoustic environment.
Measurements in a working ICU would be highly disruptive to patients and staff.
Therefore, factors were assessed by taking measurements in a laboratory furnished to resemble a 4-bed ICU. Each patient area included a bed and furniture such as chairs, cabinets and stands. A multiple-nurse’s desk was installed in the space, equipped with multiple chairs and monitors.
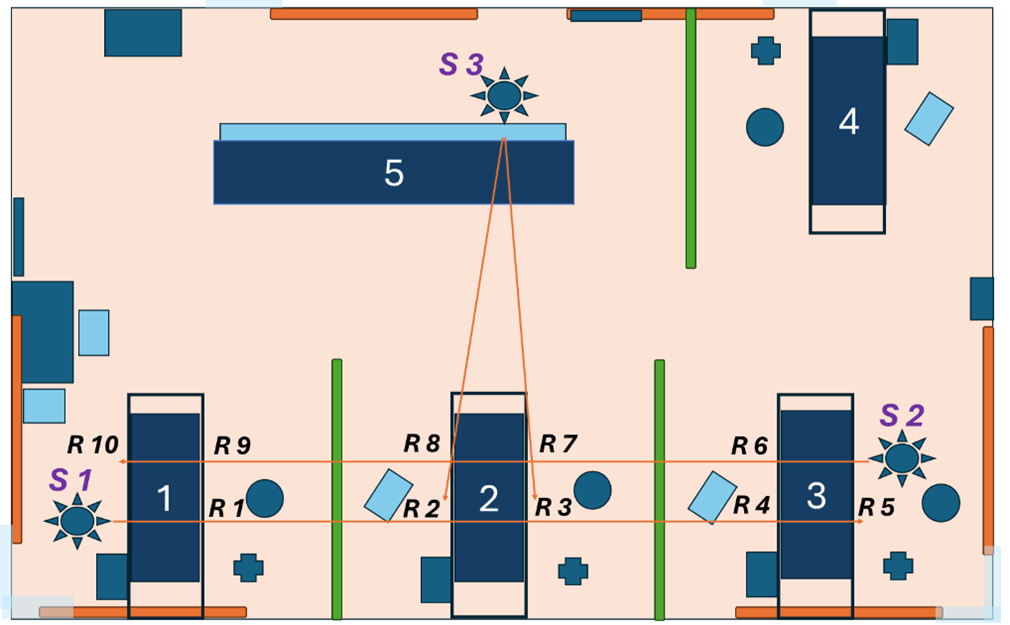
The location of screens is highlighted in green and wall panels in orange.
Methods
Impulse response measurements were used to capture:
- Reverberation Time (T20)
- Clarity (C50)
- Speech Transmission Index (STI)
- Spatial Decay of Speech (D2,s)
The privacy conditions of a patient in the middle bed (Bed #2) were assessed in reference to speech coming directly from the nurse’s desk as well as from the adjoining bedside. The STI was recorded assuming that a lower value would suggest better conditions for speech privacy.
Testing within a laboratory allowed different room configurations and setups to be installed, and the effect of room treatment, such as acoustic ceiling tiles and wall panels.
Additionally, 3 different screen partitions between the beds were tested:
- Office Screens (Ecophon Akusto)
- Hospital Screens (Silentia AB)
- Polymer Curtains (Specialgardiner AB)

Results & Discussion
Speech intelligibility improved
With the addition of acoustic treatment, room conditions are much improved and better suited for speech intelligibility, with an overall improvement from Fair/Good to Excellent conditions even for the case with no screens installed.
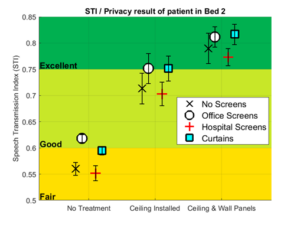
The hospital screens lend themselves to good privacy conditions. Adequate RT times of below 0.6 seconds can be achieved with this screen when used in tandem with both the ceiling and wall panels. Compared to the other screens tested, the hard reflecting nature of the hospital screens results in a reduced clarity value, degrading the intelligibility, which may improve the condition for speech privacy.
When assessing these spaces using the open plan office metrics, not one of the setup combinations satisfied the example values listed in the standard that indicate good acoustic conditions. In this case, a spatial decay of greater than 8 dB.
It is worth noting, however, that these intelligibility and privacy tests were performed in the absence of background noise, the addition of which would certainly worsen the conditions for speech yet improve them for the sake of privacy.
From this preliminary study, further investigation into adding noise and the resulting degradation in STI and improvement in privacy would be useful. Additionally subjective test to investigate the relationship between speech intelligibility, privacy and annoyance.
References
[1] Johansson L, Knutsson S, Bergbom I, and Lindahl B. (2016). Noise in the ICU patient room – Staff knowledge and clinical improvements. Intensive and Critical Care Nursing. Aug;35:1-9
[2] Ryherd, E. E., Moeller, M., Jr., and Hsu, T. (2013). Speech intelligibility in hospitals. The Journal of the Acoustical Society of America, 134(1), 586-595
This research was conducted in the MSc course in Engineering Acoustics at the Technical University of Denmark (DTU), under the supervision of a Ph.D. and Associate Professor Cheol Ho Jeong. The findings were also presented at the DAS/DAGA conference in Copenhagen in March 2025. The project was done in collaboration with Saint-Gobain Ecophon.
Author: Mr. Conn Aiken
Email: [email protected] Phone +45 5023 18 20

