
Increased need for Dementia Clinics
Demographic changes across the globe lead to higher life expectancy in general and we are facing a future where people live longer than before. We have more and more patients of higher age in our healthcare facilities, as well as Dementia Clinic, today than we used to and we need to consider this when building and refurbishing rooms that should support communication and care for all age groups. Globally, the number of people living with dementia will increase from 50 million in 2018 to 152 million in 2050, which in total is a 204% increase.
As we age, we will be challenged by hearing loss and other age-related conditions. A symptom connected to dementia is noise sensitivity which can lead to confusion, anxiety, and increased stress levels. Physiological reactions to noise are increased heart rate, high blood pressure and heavy fatigue. Social isolation can be the result of a lack of hearing and understanding of what is said. The relationship between people with dementia and their physical environment and a building/room can have a therapeutic effect on people with dementia if it is well-designed.
Dementia clinic in Aarhus
The dementia clinic in Aarhus (Denmark) is an outpatient clinic that serves for cognitive testing of patients who will visit for a short while, approximately 1 hour. Training and testing take place and there is no social interaction with other patients.
The examination room depends on good communication between staff and patients as the purpose often is to evaluate the patient’s cognitive status. The examination room was perceived as problematic as the poor acoustic quality possibly interfered with the patient’s ability to hear the questions and instructions from the examiner.
Refurbishment
The examination room went through an acoustic refurbishment. Before, the room had a plasterboard ceiling that was then altered to a 20 mm thick glass wool acoustic absorber with a painted surface with a total area of 16m2, corresponding to floor area. Due to the limited ceiling height, the absorbent ceiling had to be directly fixed (glued) to the soffit instead of suspended and placed in a grid. The lack of air between the absorber and the soffit makes the absorption lower than if we could have had the recommended suspension of 200 mm. No other changes to the room were made.
Measurements
Reverberation Time (RT)
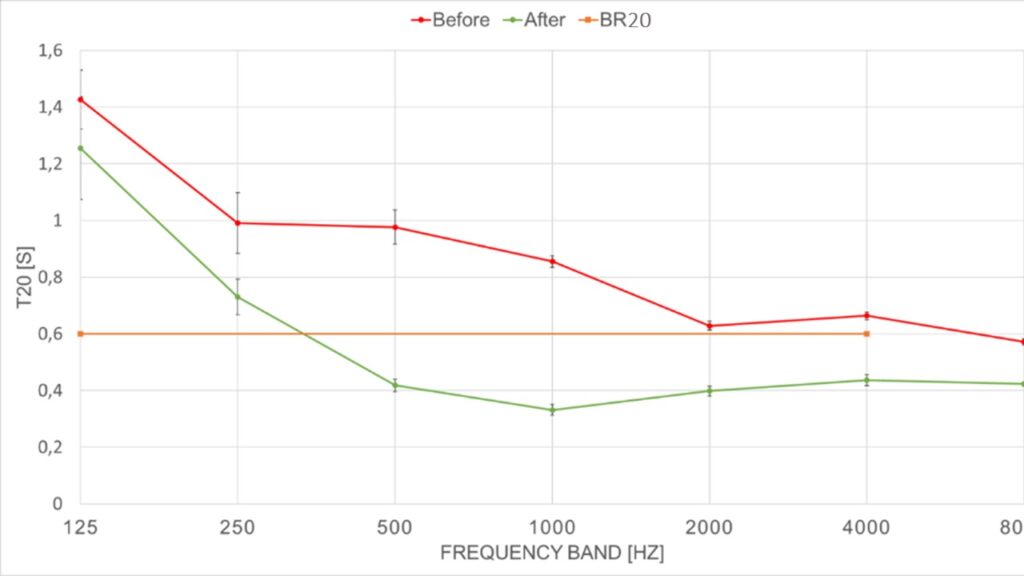
Reverberation time is defined in ISO 3382-1 (2009) as the time it takes for a sound source to drop 60 dB in level and is in this study evaluated in T20. In Figure 1 measurements before and after acoustic refurbishments are displayed. A substantial reduction of reverberation time was observed in all frequency bands, and this is very beneficial and noticeable in the mid-spectrum which is important for human speech comfort. The average RT was lowered from approximately 0,9 sec. to 0,6 sec. (125-4000 Hz) thus meeting the Danish standard (BR20) for examination rooms. This suggests a noticeable change for staff and patients, however, perhaps not enough for patients with hearing disabilities.
Speech Clarity (C50)
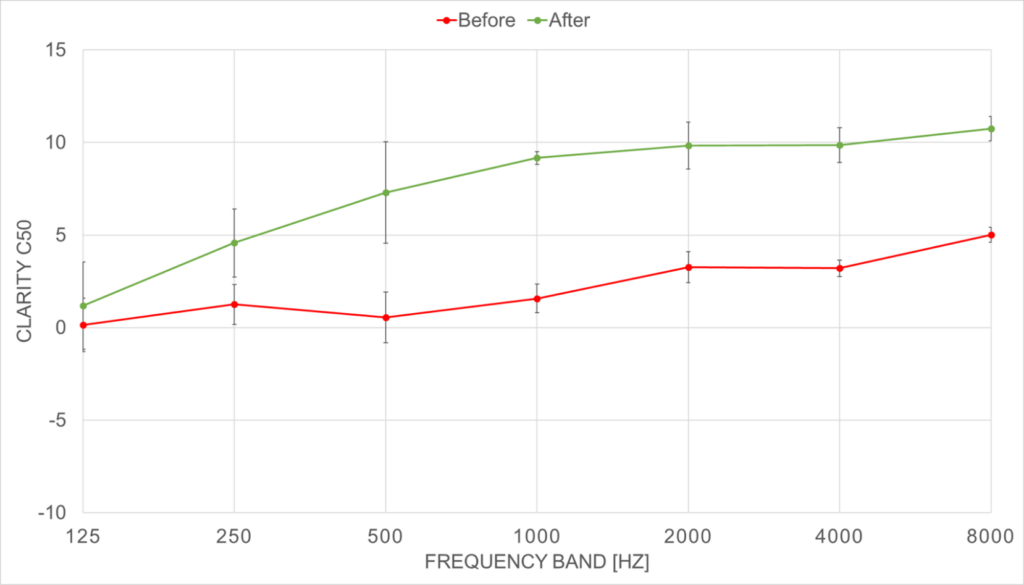
In Denmark, the demands for elderly care rooms unfortunately only include reverberation time. Whereas Clarity of speech, C50 is a relevant descriptor when evaluating a room for communication. As defined in ISO 3382-1 (2009) C50 evaluates the ratio between the early sound reflections, within the first 50 milliseconds, and the total sound energy. As a rule of thumb: the higher the value of C50 (evaluated in dB) the better the clarity of speech in a room. In Figure 2 the before and after measurements show a large improvement after refurbishment. Speech clarity increases from very low values to between 5-10 dB in most frequency bands. This indicates a very good level of speech clarity and comfort for the people communicating in the room.
Speech Transmission Index (STI)
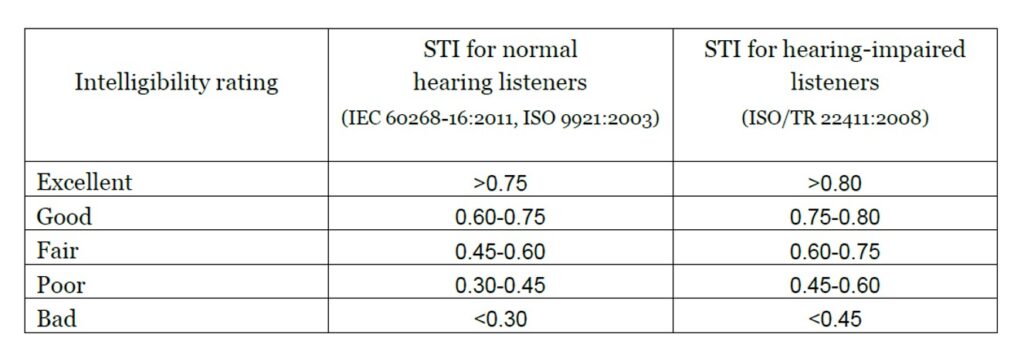
Speech Transmission Index is a measure of speech transmission quality more related to listener perception. It measures the quality of speech transfer from speaker to listener. It is a numeric value that varies from 0 = bad to 1 = excellent (Table 1). STI predicts the likelihood of syllables, words and sentences being comprehended. The values in the dementia clinic changed from 0,66 (good) to 0,81 (excellent) after the intervention, applicable to a normal-hearing person. If the patient suffers from a hearing impairment, highly likely due to the patient’s age, this would instead be changed from fair to excellent. The impact on the patient´s ability to accurately hear what is being said is substantial.
It is hard to conclude whether the Danish target value (0,6 seconds) for T20 is ‘good enough’ to secure a supportive sound environment for elderly care and dementia care but there is a trend in the questionnaires showing that lower reverberation time together with higher C50 and STI are preferable. The ‘after’ results in the questionnaires reveal that staff scores the facilities better after the acoustic refurbishments and the measurements support these findings.
Dementia assessment clinic conclusion
In this dementia clinic, the ‘after’ results do not meet the Danish standard. On both 125 and 250 Hz the values still exceed the standard demands (Figure 1) after the refurbishment but according to the questionnaires, the impact of the change of acoustics on the end-users is highly positive. If we didn’t have the questionnaires but chose to include more acoustic descriptors than just reverberation time both C50 and STI could support what we already know from the questionnaires.
This paper and work have demonstrated that this dementia care facility was insufficient when it comes to room acoustic quality. The before measurements together with the questionnaires showed that the room was challenged on reverberation time, speech clarity and speech transmission index. The fact that Danish standards don’t include several acoustic descriptors is problematic since reverberation time only shows one aspect of a room and therefore doesn’t always take the activity into account.
Acoustic treatment must be done to the room geometry, the activity in the room and the people using the room
Acoustic treatment must be done to the room geometry, the activity in the room and the people using the room – one size does not fit all. The after-measurements show improvement in all acoustic parameters, as well as, the subjective experiences expressed by physicians in the survey. A minor refurbishment can deliver noticeable improvement.

The study was presented at ARCH24 The 6th International Conference on Architecture, Research, Health, and Care, at Aalto University, Finland, 17-19 June 2024.
More reading:
Age-related hearing loss and acoustics
The importance of acoustics in designing spaces for people with dementia
If you are interested in more details please reach out to the author Maria Quinn

